Floretina
Image banks
Send your image banksThis image may not be copyrighted, but is credited to the author(s) and the download and use of the images are for informational and non-commercial use If used in presentations the following credits should be mentioned: Copyright notice: “This image was published in the FLORetina.com website, Author, Title".
Search in image banks section
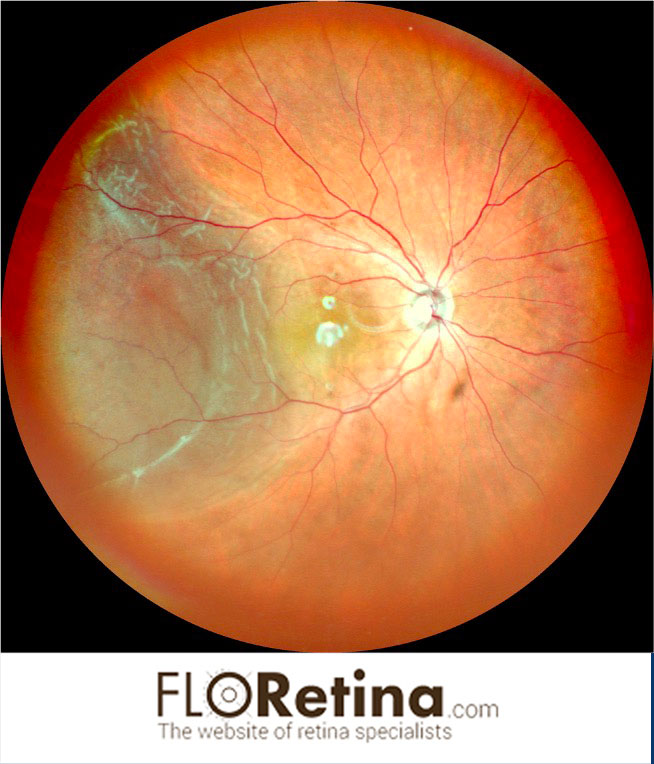
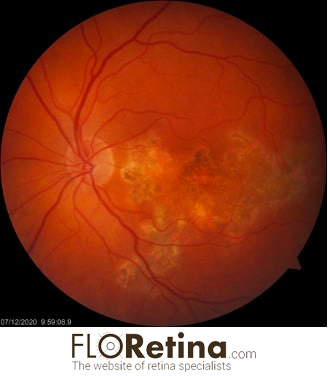
Rickettsial retinitis
SHARAN NALWARRickettsial infections are caused by a variety of obligate intracellular, Gram-negative bacteria. Ocular involvement is common but often asymptomatic. All ocular structures can be involved, but posterior segment involvement is more common and most severe. Common posterior segment manifestations are inner retinitis with associated vasculitis and mild vitritis. There are various speculations regarding the pathogenesis of rickettsial retinitis. The cotton wool spot-like retinal lesions could result from intraretinal multiplication of organisms or alternatively due to immune complex deposition along retinal vessels.
View imageLetrozole-induced unilateral acute intermediate uveitis with cystoid macular edema
SHARAN NALWARA case of 48 y/o lady who presented with DOV in RE (6/60) since 15 days. She had a h/o Ca right breast treated with mastectomy 13 years back & was prescribed letrozole(AROMATASE INHIBITOR) 2.5mg OD as she had tested ER +ve. Anterior segment showed cells in AC & anterior vitreous face. Posterior segment revealed disc & macular edema. OCT also showed disc edema & CME. LE examination was WNL. Systemic investigations were WNL. She was asked to stop letrozole after oncology consultation & was prescribed topical prednisolone & nepafenac. Discontinuation of letrozole improved visual acuity to 6/18 within 1 month.
View imageRetained iofb presenting as vitreous haemorrhage
SHARAN NALWARPatient presented with dimunition of vision in right eye,on evaluation patient had re- vitreous haemorrhage,on imaging iofb noted. Planned ppv and metallic iofb removed with the help of maxgrip forceps, through port widening,procedure uneventfull
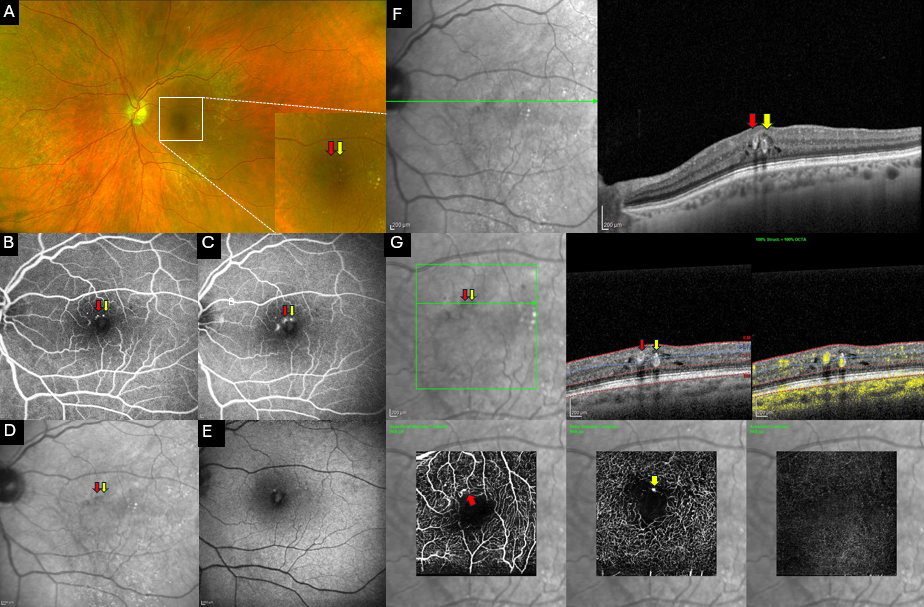
View imageMultimodal imaging of Perifoveal Exudative Vascular Anomalous Complex (PEVAC)
Francesco Barca Lorenzo De Angelis Dario Giorgio Benedetta Pieri Veronica DonatiMultimodal imaging showing PEVAC in the LE of a 73-year-old woman. The patient did not exhibit any clinical signs of diabetic retinopathy, hypertensive retinopathy, retinal vascular occlusion, or myopic degenerative retinal disease. (A) Ultra-wide field fundus imaging showing perifoveal isolated aneurismal lesions ( magnified imaging in the bottom) barely visible on color photography. Drusenoid lesions are detectable in the mid-periphery. (B,C) Fluorescein angiography (FA) reveals well-defined hyperfluorescent lesions well detectable in the (B) early phase with leakage in the (C) late frame. (D) These lesions appear as hyporeflective spots on IR imaging. (E) An increase of the autofluorescence signal is detectable on B-FAF at the macula. (F) Structural OCT examination passing through the lesions showing the presence of an isolated, well-defined perifoveal aneurysmal lesions with a hyperreflective wall (red and yellow arrowhead) and surrounding intraretinal cystic spaces. (G) OCT-angiography confirming the presence of perifoveal capillary abnormalities (green line) in the superficial (red arrow ) and deep capillary plexus (yellow arrow) and a mild rarefaction of retinal capillaries in the perilesional area in both the plexi. No abnormalities are detectable in the avascular slab. More specifically, corresponding B-scans with flow overlay clearly disclose an isolated large dilation (red and yellow arrows) corresponding to PEVAC with detectable flow inside the lesions
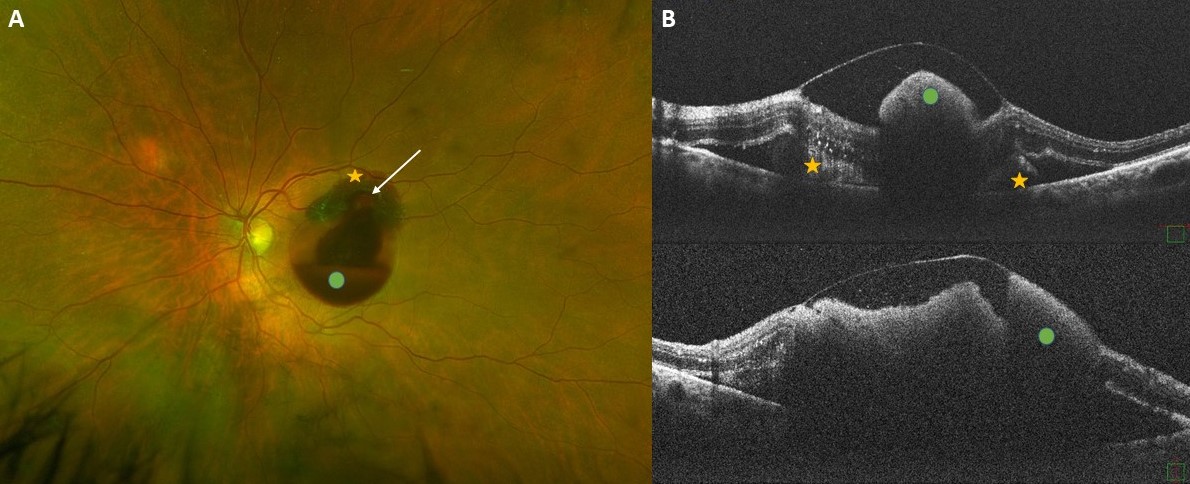
View imageImaging of a retinal arterial macroaneurysm
Francesco Barca Lorenzo De Angelis Bianca Pacini Mario Galasso Dario Giorgio(A) Ultra-widefield fundus imaging shows a case of a 74-year-old woman with a ruptured retinal arterial macroaneurysm (white arrow) in the left eye. Preretinal (green dot) and subretinal hemorrhages (yellow asterisks) are visible at the posterior pole. (B) Optical coherence tomography examination obtained in the acute phase shows large amount of sub-inner limiting membrane hemorrhage (greendots) with outer-layer shadowing, subretinal hyperreflective material (yellow astetisks) and a pocket of subretinal fluid.
View imageBilateral papilledema associated with retinal hemorrhagic appearance as earliest sign of spinal cord tumor
Federico GiannuzziA 57-year-old obese patient admitted to our ophthalmic department complaining of bilateral sense of eye swelling and mild blurring vision. The anterior segment and pupillary reflex were normal on ophthalmological testing. Likewise, eye movements were preserved and she did not report diplopia in any position of gaze. Dilated fundus examination revealed bilateral hemorrhagic papilledema, pre-retinal hemorrhages in both eyes, dot and blot hemorrhages in the peripheral retina. Visual acuity was 20/20 in both eyes. Routine hematological investigations revealed increased both Von Willebrand factor and ristocetin factor and LAC positivity. The lumbar puncture (LP) showed elevated cerebrospinal fluid (CSF) proteins. Magnetic resonance imaging (MRI) with contrast of brain and spinal cord showed signs of intracranial hypertension and the presence of two lesions in continuity with each other respectively located at T12-L1 and L1-L2. Radiologic features were compatible with the diagnosis of ependymoma. A surgical procedure was conducted and confirmed the diagnosis after anatomical pathology analysis.
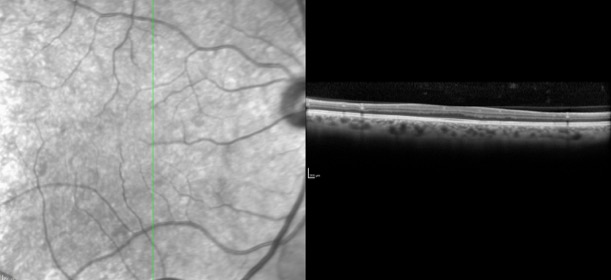
Isolated Foveal Hypoplasia
Ilkay Kilic MuftuogluA-60-year-old female patient without remarkable ocular and/ or systemic history referred for a routine eye examination. Best corrected visual acuties were 20/25 in both eyes. SD-OCT scan cutting through the center revealed lack of foveal pit. In OCT-A slabs, FAZ was not appreciated at superficial and deep capillary plexus levels. She was diagnosed as isolated foveal hypoplasia.
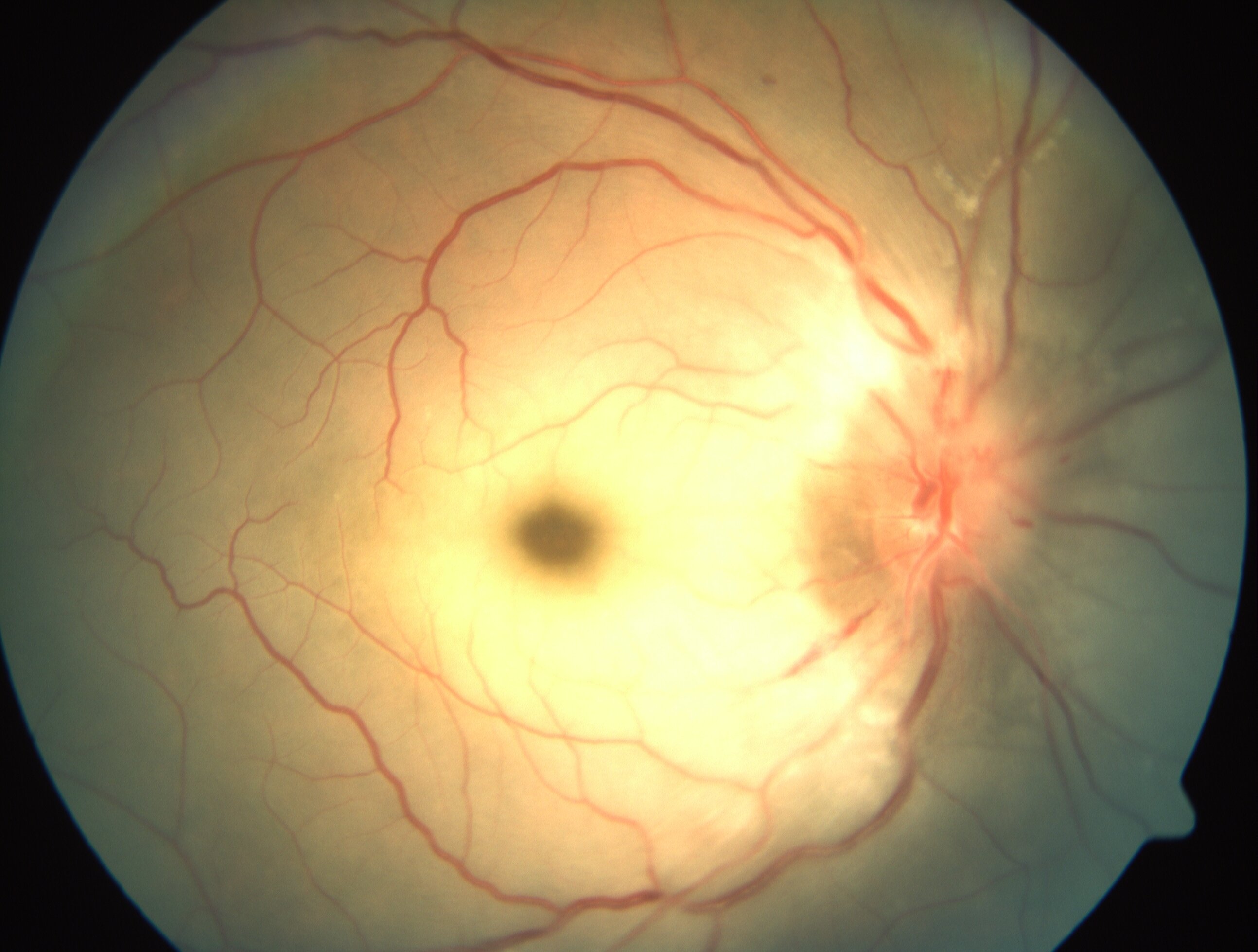
View imageCentral retinal artery occlusion
Dr Pavithra SubramaniyanCentral Retinal Artery Occlusion with Hypertensive Retinopathy
View imageDr.
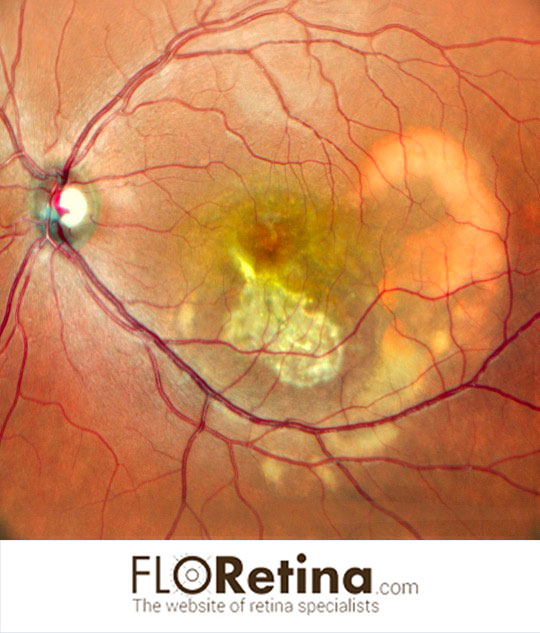
Fendouli Ines Zouara Hajer Rahma Saidane Chebbi Amel Bouguila HediWe report the case of an uncomplicated choroidal osteoma in a 27-year-old woman, with no medical history, presented to our department with sudden onset visual loss in her right eye (RE). Opthalmological evaluation revealed a best corrected visual acuity of 4/10 and normal anterior segment in the RE. Fundus examination revealed a slightly elevated, round shaped, yellowish-orange coloured lesion. Choroidal osteoma is a rare and benign ossifying tumor, affecting mostly Caucasian females, in early twenties. This affection is often unilateral, occurring in an apparently healthy eye. It is generally located in juxta or peri-papillary areas. Diagnosis is based on clinical examination, aided by multimodal imaging, including optical coherence tomography (OCT), OCT-angiography and ultrasonography. Choroidal neovascularisation represents its main complication.
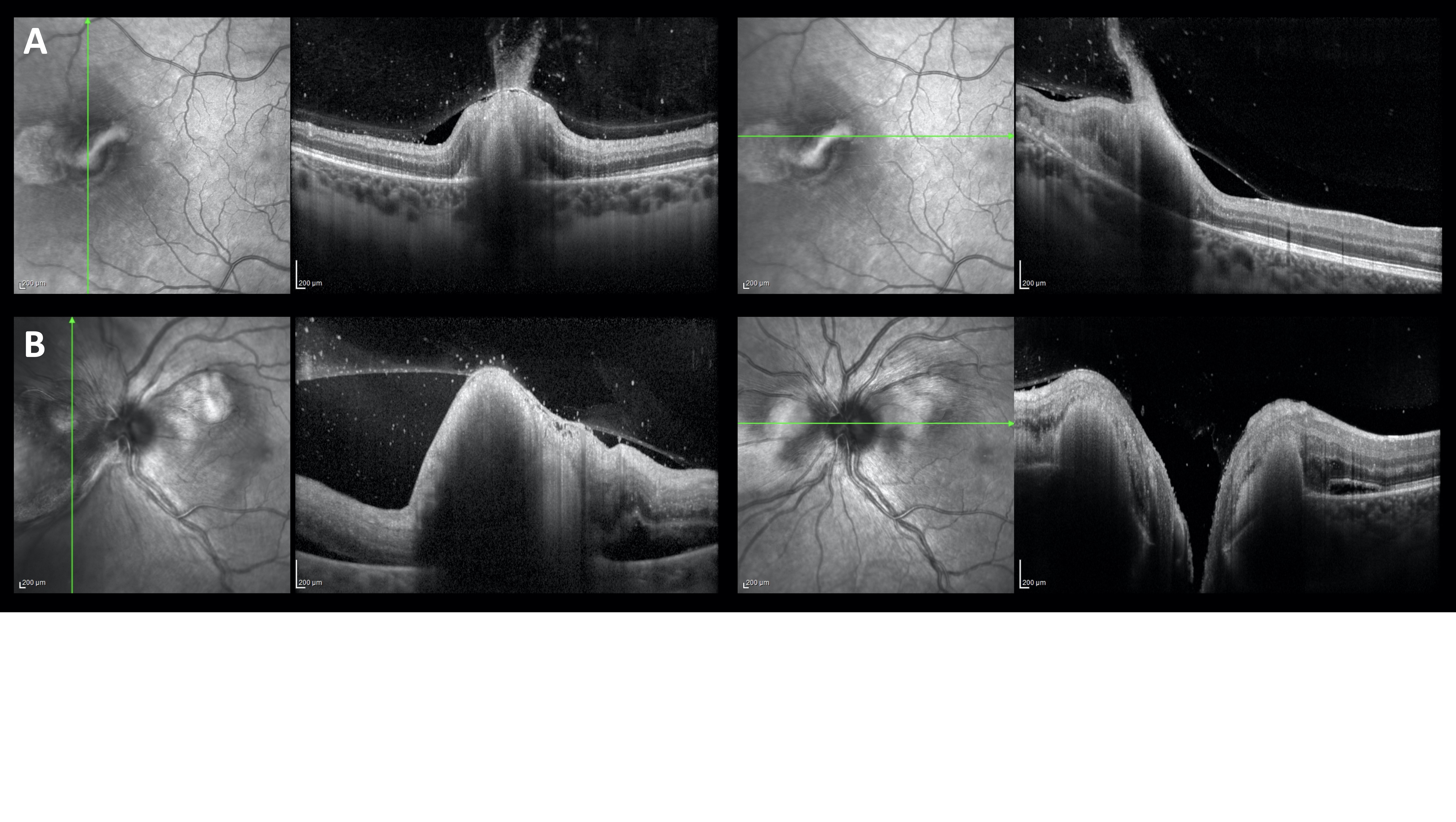
Bilateral Candida albicans chorioretinitis
Andrea SaittaA case of an immunocompromised 30-year-old woman with bilateral Candida albicans chorioretinitis. (A) In the right eye structural OCT shows a highly reflective lesion involving the full-thickness retina and protruding into the vitreous. The hyperreflective dots in the posterior vitreous are infiltrating inflammatory cell. (B) In the left eye structural OCT shows two juxtapapillary lesions originating at the retinal pigment epithelium/choroid layer and penetrating into the neurosensory retina. Subretinal fluid is present. The hyperreflective dots in the posterior vitreous are infiltrating inflammatory cell.
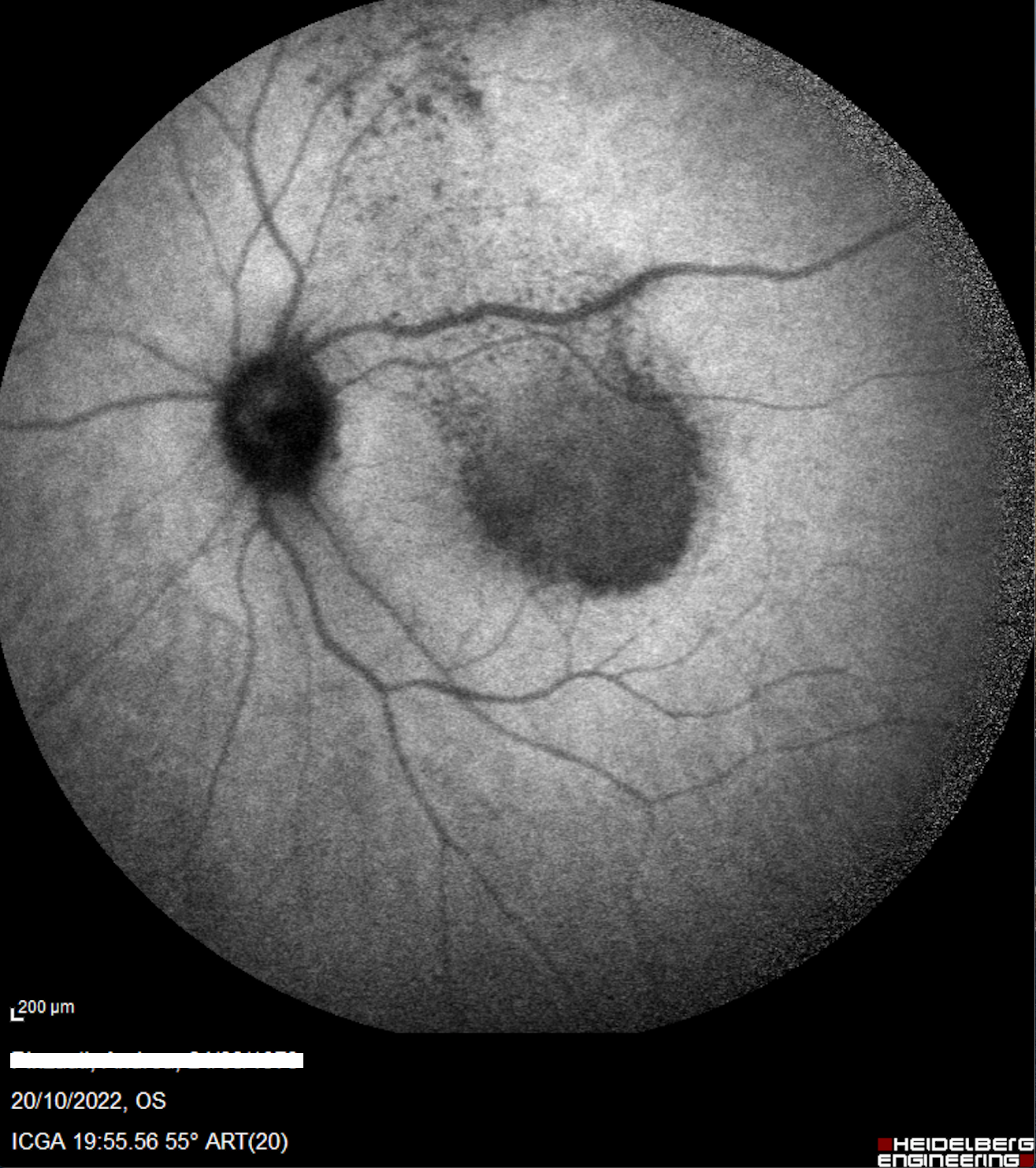
View imageSyphilitic posterior placoid chorioretinitis
Daniela Bacherini Giovanni Romualdi Fabrizio GiansantiA case of 49 y.o. man, caucasian, with no history of drugs and systemic disease, referred to our emergency room due to a sudden para central scotoma in his left eye. Our multimodal imaging allowed us to diagnose a syphilitic posterior placoid chorioretinitis, confirmed few days later with serological exams (qualitative TPHA +).
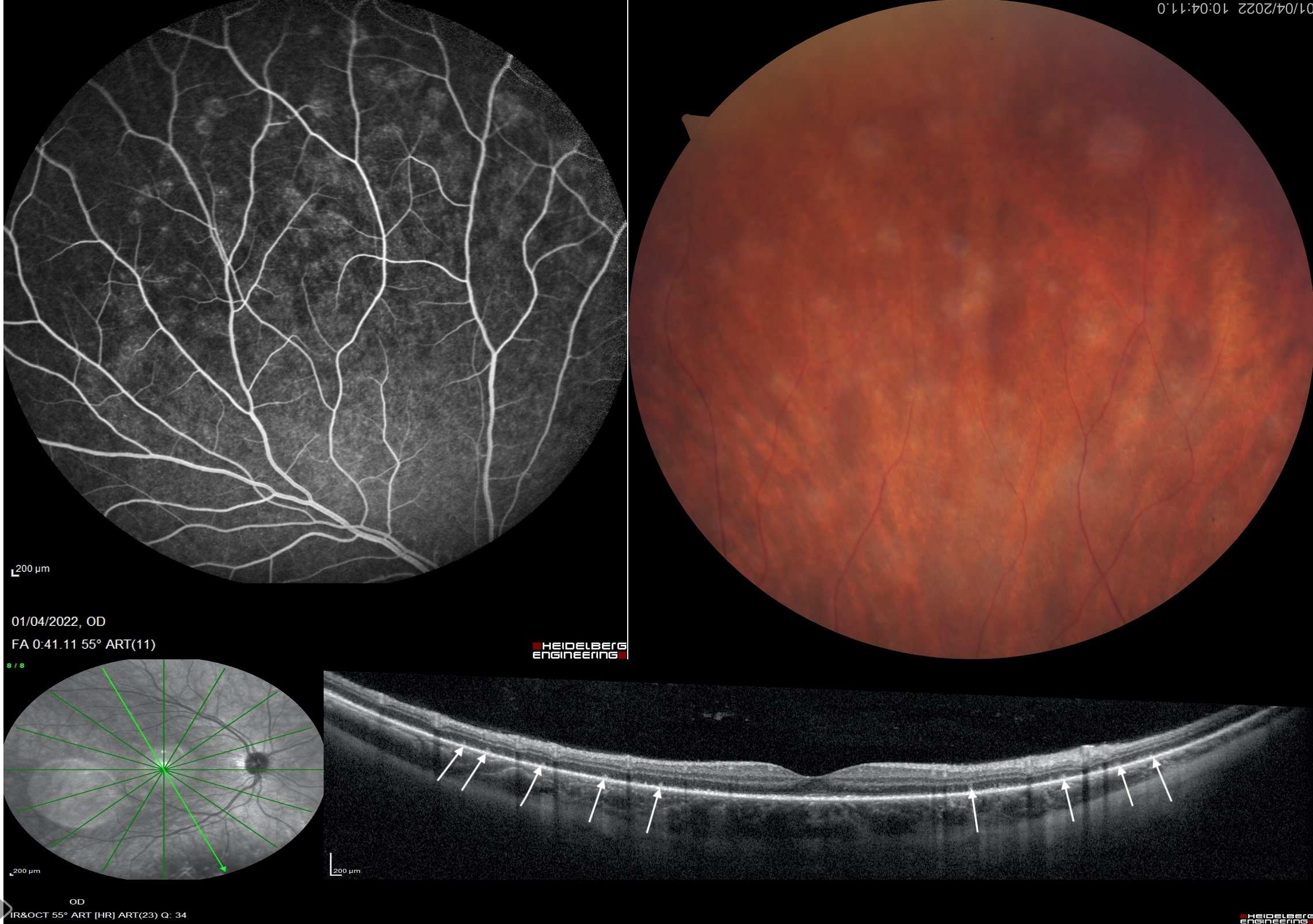
View imageMULTIPLE EVANESCENT WHITE DOT SYNDROME.
Giovanni Romualdi Daniela BacheriniA case of 24-year-old woman with MEWDS. Structural OCT shows the loss or damage of the outer photoreceptor segments (white arrows). Hypocyanescence of the ICGA is present in the intermediate angiographic phase and most clearly detected in the late phase.
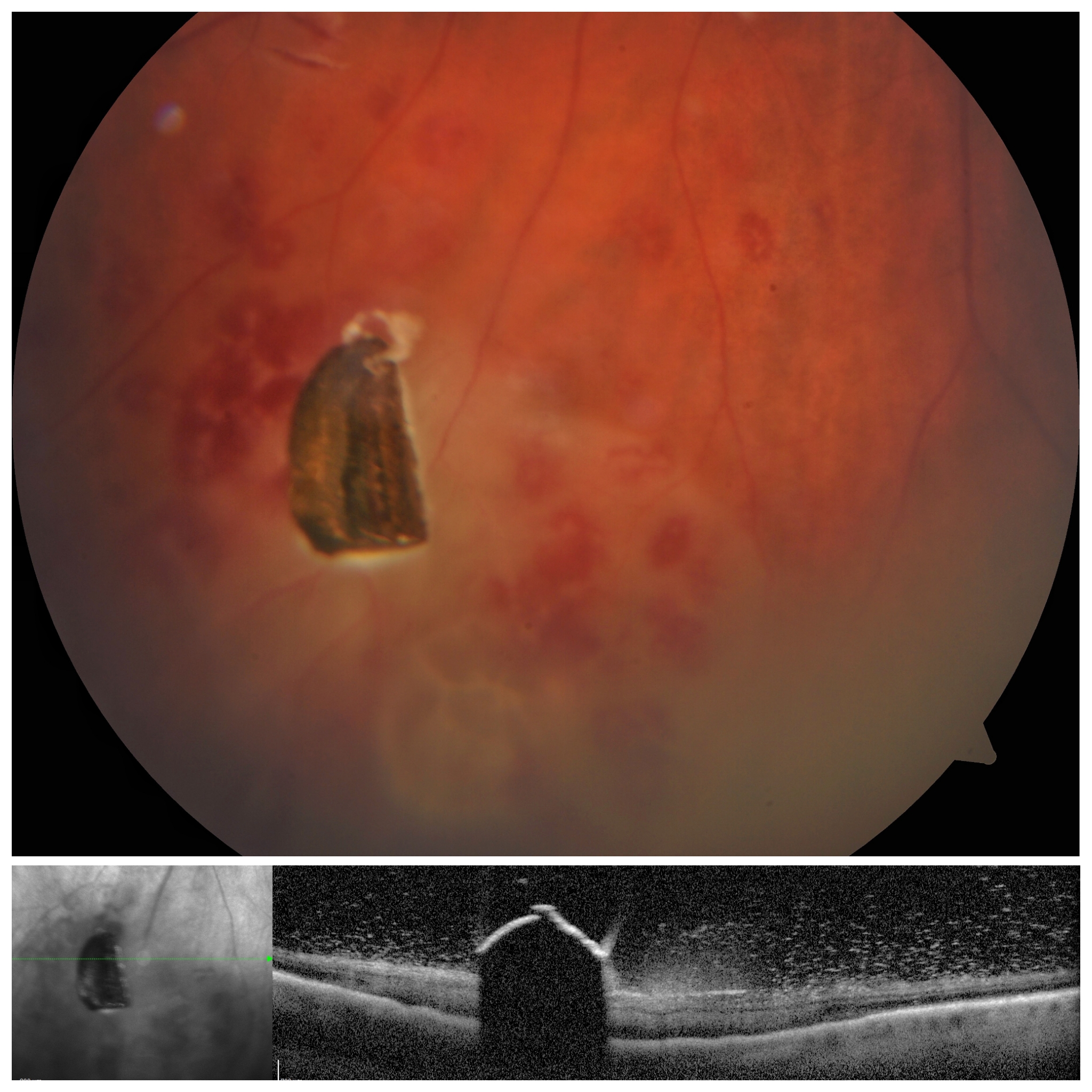
View imageMetallic Intraocular Foreign Body
Simone Stefanini Edoardo Traniello Gradassi Noemi LombardiMetallic Intraocular Foreign Body with surrounding retinal hemorrhages and vitreitis. Fundus fotograph (Zeiss), structural OCT (Heidelberg)
View imageSickle cell anemia
Andre Maia21 yo female with sickle cell anemia. Panoramic angiography shows areas of diffuse extravasation by neovessels in the retinal periphery, in addition to areas of hypoperfusion compatible with ischemia. DEVICE: California (Optos).
View imageRPE tear
Daniela Bacherini Fabrizio GiansantiImaging device: A. Color fundus photography, angle 89°, Nidek, B. retromode
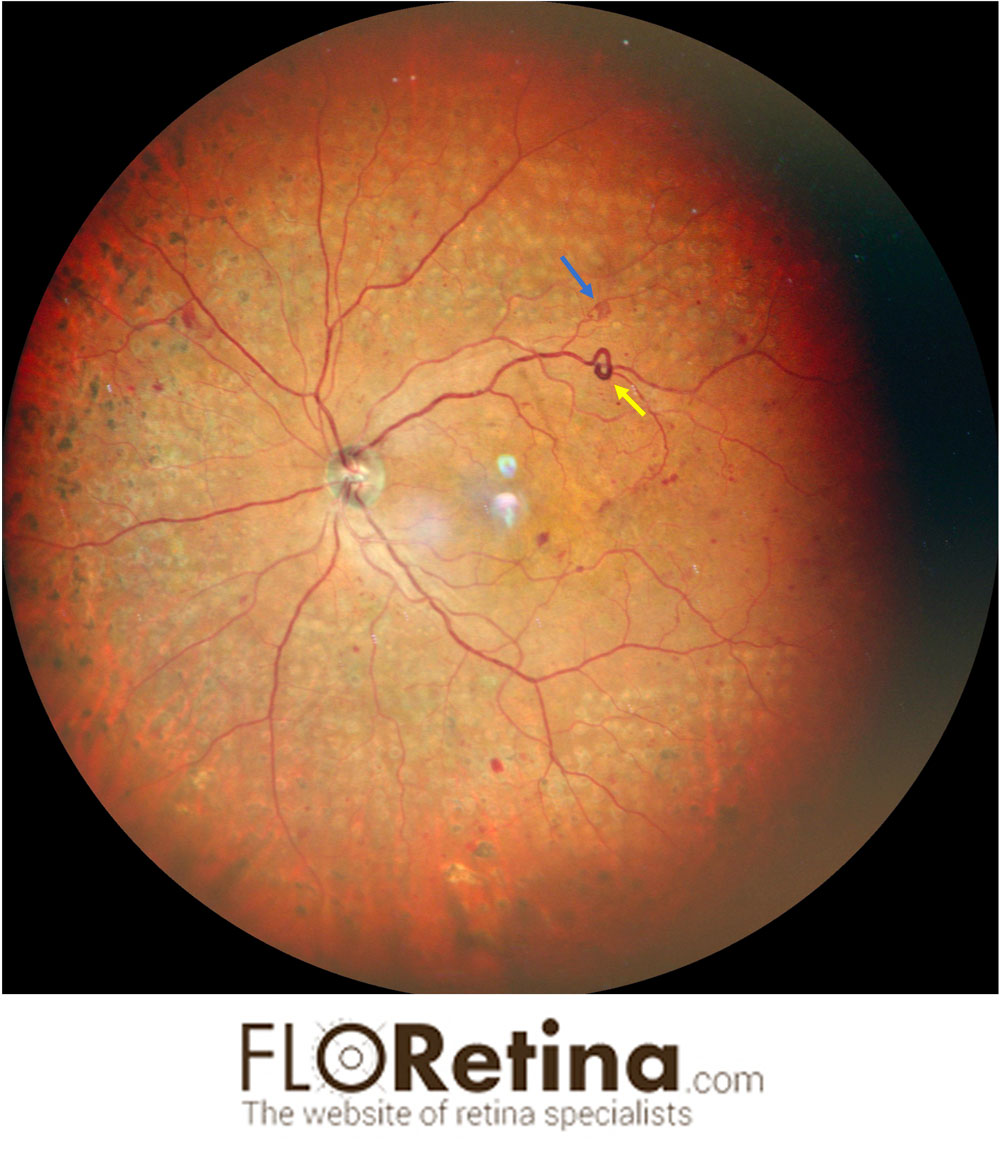
View imageProliferative Diabetic retinopathy
Daniela BacheriniDescription: 45 Y/O male with proliferative diabetic retinopathy treated with laser. A retinal neovessel (blue arrow), Intraretinal Microvascular Abnormality (IrMA) (yellow arrow) are evident
Imaging device: Ultrawidefield color fundus photograph 163°, Nidek
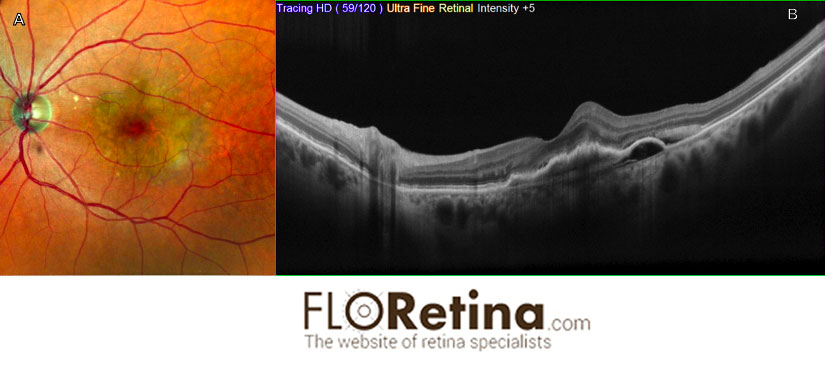
Neovascular AMD
Daniela Bacherini Francesca CipolliniImaging device: A.Color fundus photography, angle 89°, Nidek; B. Structural OCT
View imageRetinal Detachment 1
Daniela BacheriniImaging device: Ultrawidefield color fundus photograph 163°, Nidek
View imageRetinal Detachment
Daniela BacheriniImaging device: Ultrawidefield color fundus photograph 163°, Nidek
View imageSoft drusen
Daniela BacheriniImaging device: A. Color fundus photography, angle 89°, Nidek; B. fundus autofluorescence; C. retromode DL; D. rretromode DR; E. structural OCT
View imageBilateral Soft drusen
Daniela BacheriniImaging device: Color fundus photography, angle 89°, Nidek
View imageBenign Concentric Annular Macular Dystrophy
Daniela BacheriniImaging device: Color fundus photography, angle 89°, Nidek
View imageChoroidal tubercoloma and peripheral retinoschisis
Daniela BacheriniImaging device: Ultrawidefield color fundus photograph 163°, Nidek
View imageExtramacular Best disease
Daniela Bacherini Francesca SantoroImaging device: Color fundus photography, angle 89°, Nidek
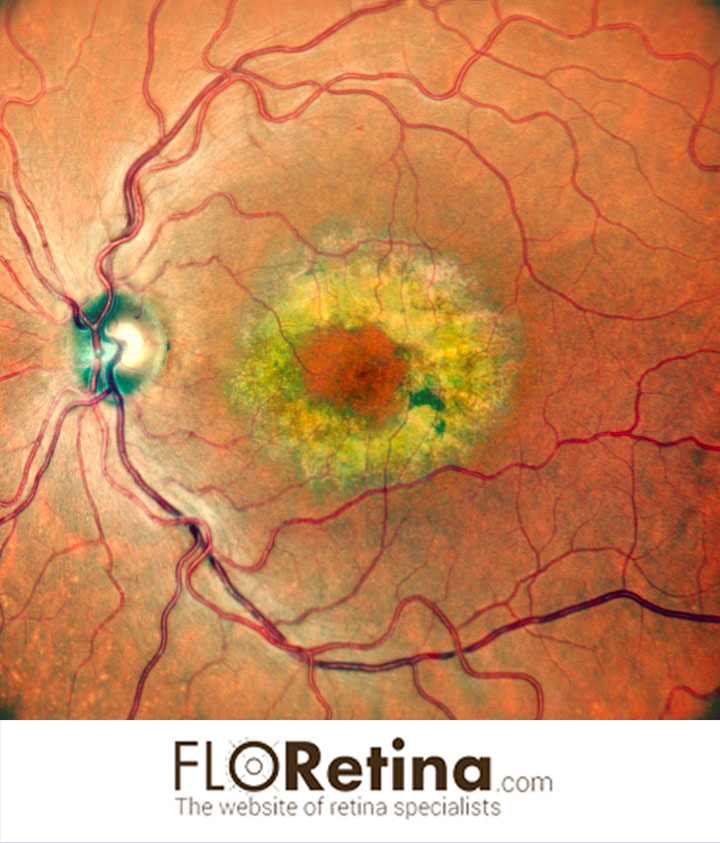
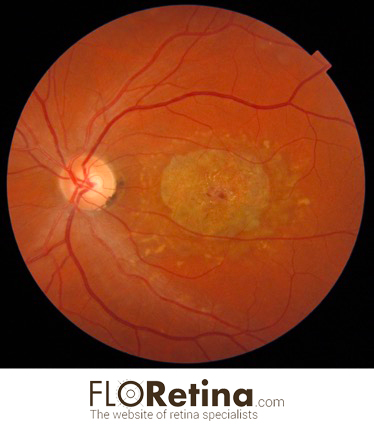
View imageCHOROIDAL OSTEOMA complicated by choroidal neovascularization
Daniela Bacherini Stefano Mercuri Fabrizio GiansantiImaging device: Color fundus photography, angle 89°, Nidek
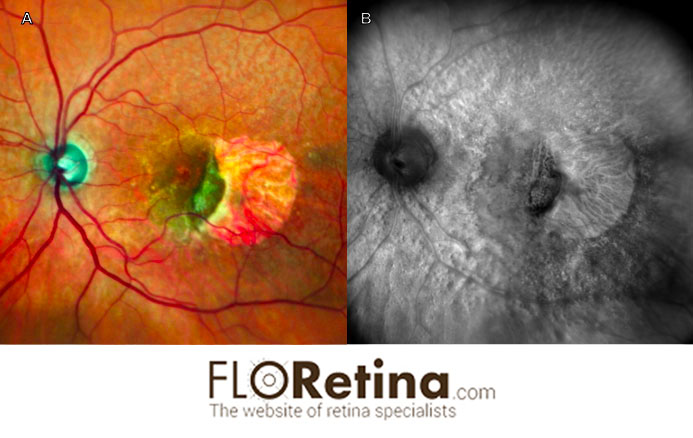
View imageRPE (retinal pigment epithelium) tear
Daniela Bacherini78 yo female with RPE tear. DEVICE: Fundus fotograph (Zeiss), structural OCT (Heidelberg)
View imageSTARGARDT DISEASE
Daniela Bacherini34 yo female with atrophic maculopathy and adjacent flecks. DEVICE: Color fundus photograph (Tocpon)
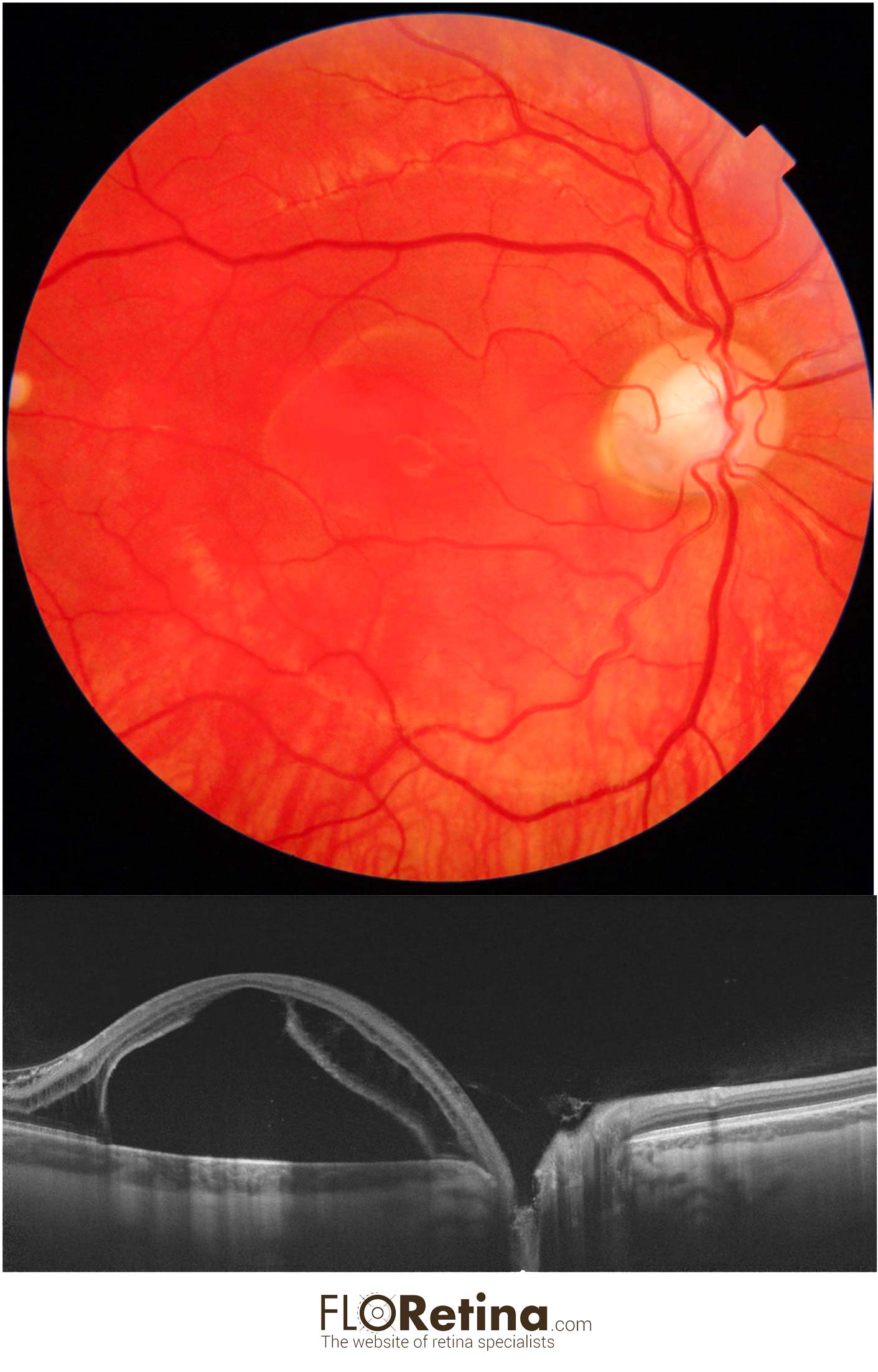
View imageOPTIC DISK PIT
Daniela Bacherini Tomaso Caporossi Alfonso Savastano25 y/o male with visual reduction showing macular schisi with detachment due to optic coloboma.
A. Color fundus photograph
B. Structural OCT showing the retina splitted at both the inner and outer retinal layers with a macular detachment
DEVICE: Fundus photograph (Topcon), Structural OCT (Topcon)
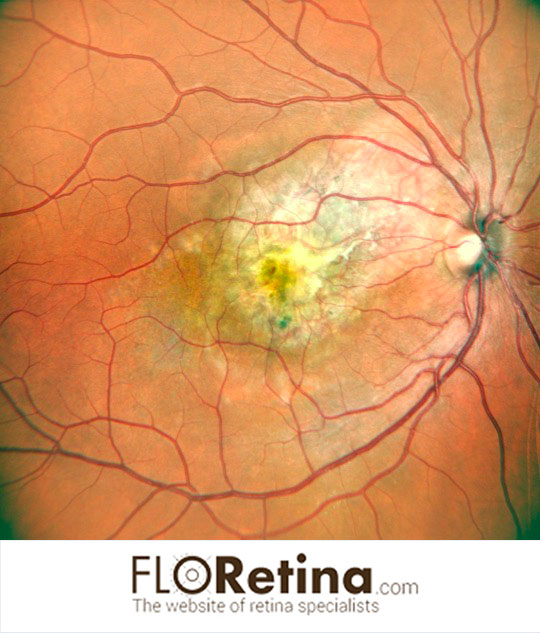
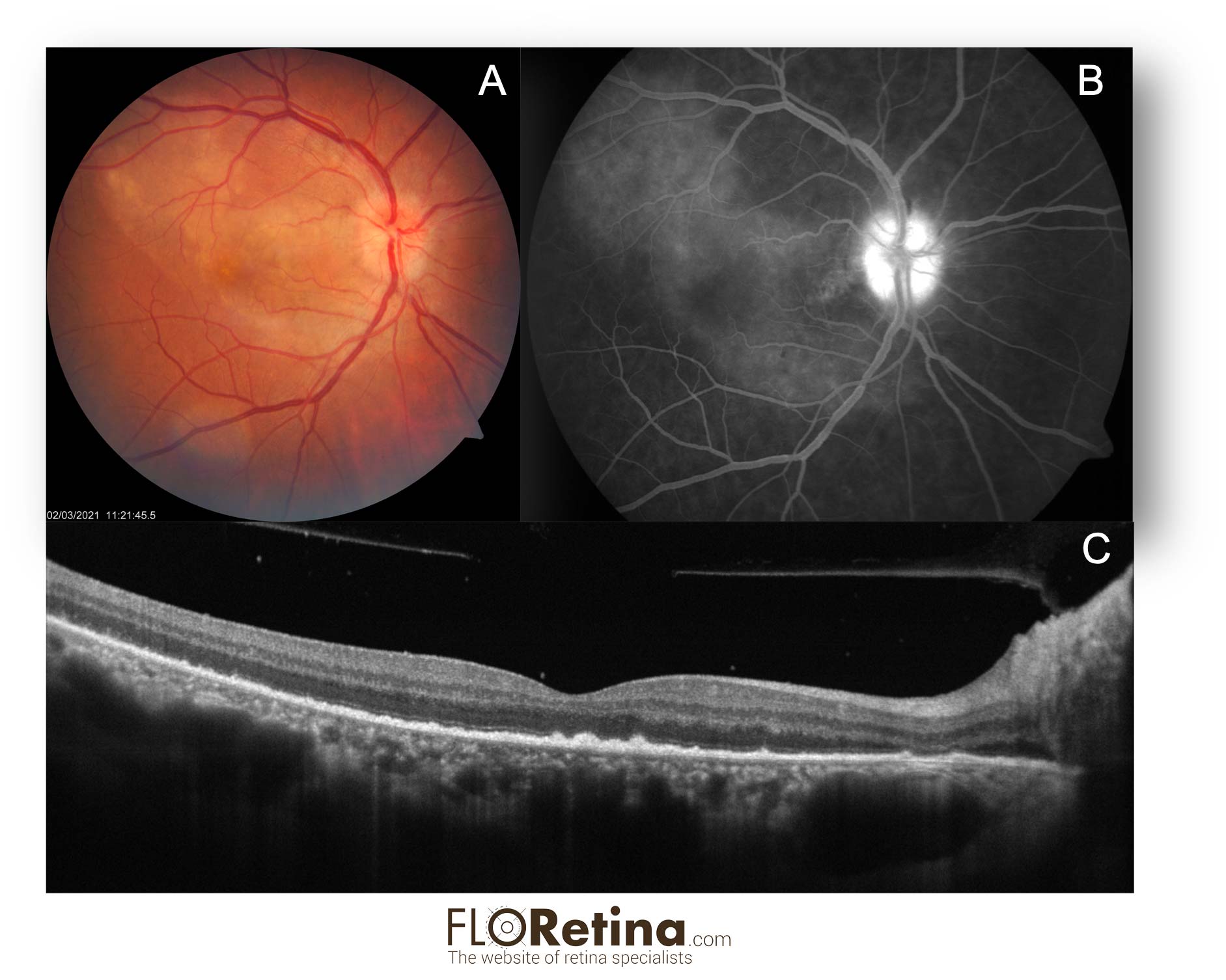
Acute Syphilitic Posterior Placoid Chorioretinopathy (ASPPC)
Daniela Bacherini Stefano Mercuri Fabrizio GiansantiA. Fundus photograph showing vast round placoid yellow zone in the posterior pole;
B. FA reveals hyperfluorescence of the optic disk with a zone of hyperfluorescence in the posterior pole (tissue staining).
C. Structural OCT shows disruption of the ellipsoid zone and hyperreflective, nodular thickening of the RPE. Hyperreflective dots representing inflammatory cells are visible in the vitreous and attached to the posterior hyaloid.
DEVICE: Multimodal imaging: fundus photograph, FA, Structural OCT
UNILATERAL ACUTE MACULOPATHY CAUSED BY COXSACKIEVIRUS
Daniela Bacherini Stefano Mercuri Federica Serino37 Y/O male with an eccentric yellow lesion (orange arrow) corresponding to a neurosensory retinal detachment. DEVICE: Fundus camera, Zeiss.
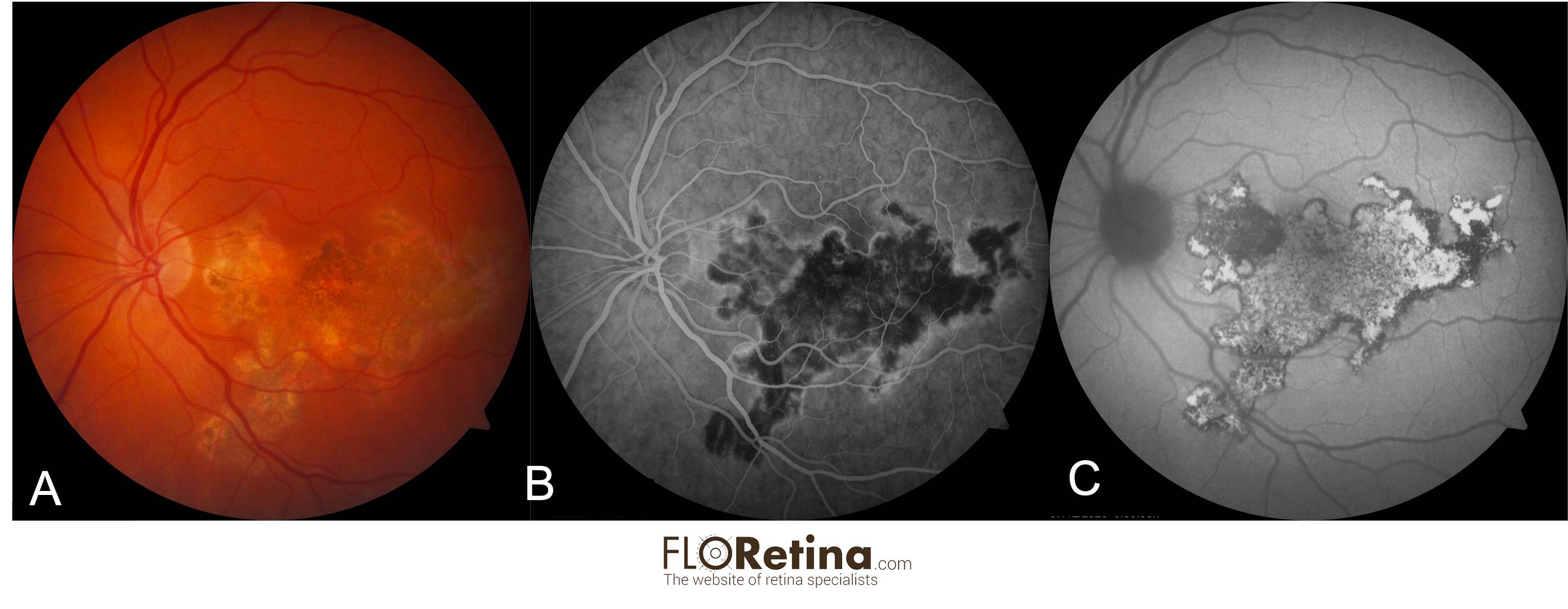
View imageTUBERCULOUS SERPIGINOUS-LIKE CHOROIDITIS 2
Daniela Bacherini Lorenzo VannozziColor fundus photograph (A) 45 Y/O female with serpiginoid lesion extending from the juxtapapillary area. Intermediate-phase fluorescein angiogram photographs (B) of the same eyes delineating the typical hyperfluorescent margins of the serpiginoid lesions. Fundus autofluorescence image (C) of the same eye, disclosing predominantly hyperautofluorescent lesion with stippled hypoautofluorescence delimited by a thin rim of hypoautofluorescence. DEVICE: Multimodal imaging: (A) Color fundus photograph (Zeiss), (B) FA (Heidelberg), (C) Fundus autofluorescence (Heidelberg).
View imageTUBERCULOUS SERPIGINOUS-LIKE CHOROIDITIS 1
Daniela Bacherini Lorenzo Vannozzi45 Y/O female with serpiginoid lesion extending from the juxtapapillary area. DEVICE: Fundus Camera, Zeiss
View image